Why yacht kits need hospital-grade discipline
Yachts add motion, heat, humidity and access constraints. Safety rests on three aligned elements: licence, insurance with domiciliary rider, and privileges explicitly listing yacht/home/hotel. Build the kit to your approved scope, not to wish-lists.
Pre-departure gatekeepers (must be true before you pack)
Scope & privileges: yacht/home settings written on your privilege list; advanced tasks (e.g., IV therapy) approved with proctor history.
Insurance: occurrence policy or claims-made with tail; settings include yacht.
Communication chain: one medical lead for updates; household/crew manage logistics only.
Evacuation plan: receiving hospital named; route and ETA rehearsed; helipad/marina options listed.
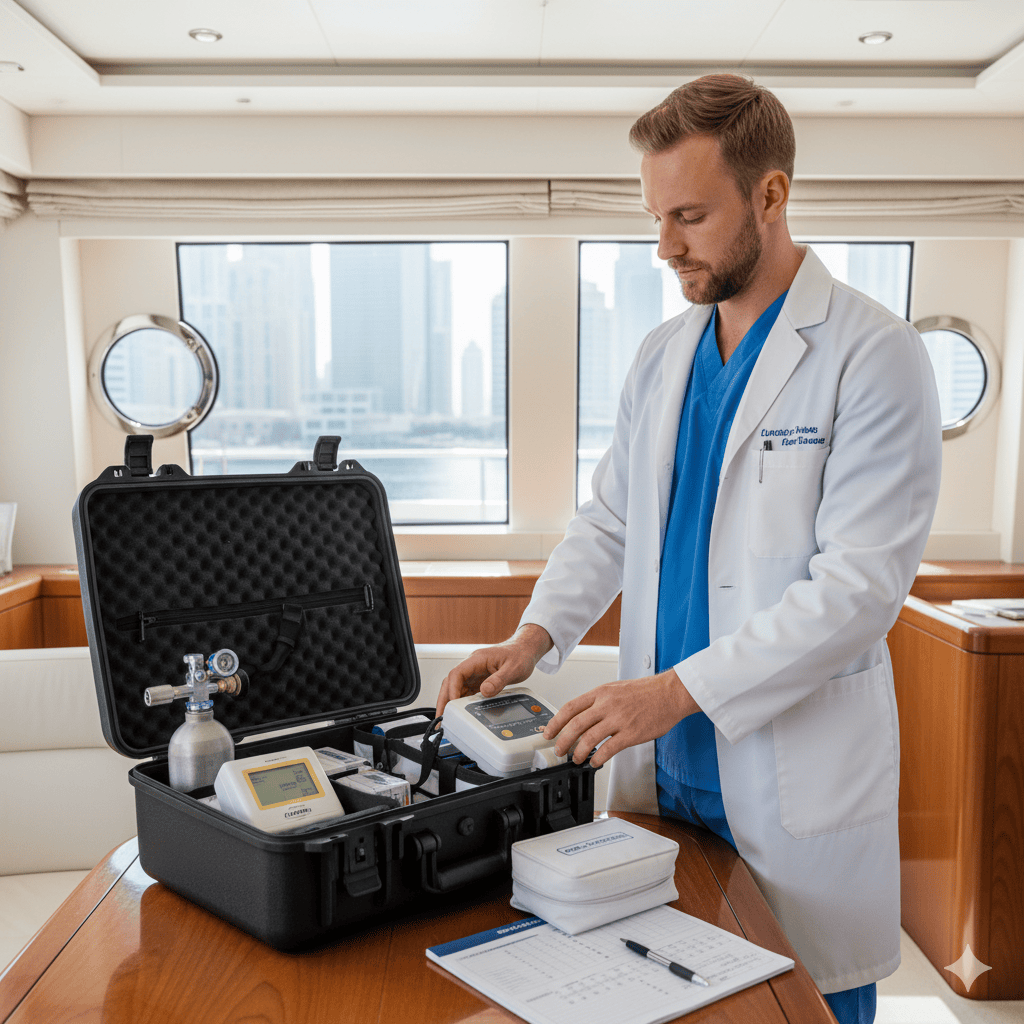
Kit architecture (tiered, copy/paste)
Tier 1 — Core first response (everyone carries)
ABHR, PPE, disinfectant wipes; basic dressings, bandages, steri-strips
Pulse oximeter, thermometer, manual BP cuff, stethoscope
Glucose gel, oral rehydration, non-opioid analgesic, antiemetic (per policy)
Epi auto-injector (where permitted), salbutamol inhaler with spacer
Small SBAR pad for numeric thresholds and time-stamped notes
Tier 2 — Procedure & monitoring (if privileged)
IV cannulas, fluids (small stock), giving sets; portable suction
Portable oxygen + masks; airway adjuncts (OPA/NPA) with sizes
Cardiac monitor/defib (AED minimum); spare charged batteries
Wound care tray; suture kit (if scope allows); sterile field supplies
Tier 3 — High-risk meds (only if insured & privileged)
Insulin, anticoagulant reversal where policy allows, concentrated electrolytes, opioids
Two-person independent double-check policy printed and packed
Temperature data logger for cold-chain items
Pack against motion: foam inserts, positive-latch cases, water-resistant containers; secure sharps/waste per maritime rules.
Custody, cold chain & documentation
Custody log: item → lot/expiry → quantity → issued/used/returned; signatures at sail and at berth.
Cold chain: insulated pouch + data logger; record temps at start/end of day.
IFUs at hand: laminated quick-refs for devices and high-risk meds.
SBAR with numbers: document escalation thresholds (e.g., SpO₂ <92% for 5 min; MAP <65) and the owner of the next action.
Infection control on board
Clean field established before patient arrival to the cabin/salon.
Waste/Sharps: puncture-proof containers; return ashore for compliant disposal.
Hand hygiene at point of care; linens in sealed bags; no mixed clean-dirty pathways.
Privacy choreography (UHNWI)
Neutral language in shared areas; doors closed; no on-screen identifiers visible.
Results and updates flow via the medical lead; no personal apps for clinical content.
Power, water & environment checks
Confirm charging for monitor/AED; carry spare batteries.
Lighting plan for procedures; headlamp backup.
Seasickness risk → antiemetic plan and spill kit.
Pre-sail checklist (10 minutes)
Privileges & insurance (yacht setting) verified
Evacuation plan printed; receiving hospital named
Oxygen level checked; AED/monitor self-test passed
Cold-chain items packed with data logger; temps recorded
High-risk meds counted; double-check process briefed
Sharps/waste pathway agreed with crew
SBAR pads and consent forms ready
Post-visit/voyage mini-audit (5 items)
SBAR note contains numeric thresholds
High-risk meds double-checked and logged
Cold-chain temperatures within range
Sharps/waste reconciled and removed ashore
Any near-miss? ≤72-hour huddle; adopt one change
Red flags—and calm responses
Unlabelled or guest-supplied meds → do not administer; escalate to medical lead.
Advanced task requested but not privileged/insured → re-scope or transfer ashore.
Power instability → switch to battery devices; shorten on-board window; prepare transfer.