Why rota architecture decides retention and safety
In premium private care, reliability beats heroics. The rota is your operating system: it determines handover quality, incident risk, and whether clinicians can sustain VIP standards without burnout. Stable patterns also shorten onboarding and make privileging decisions cleaner—because performance is predictable.
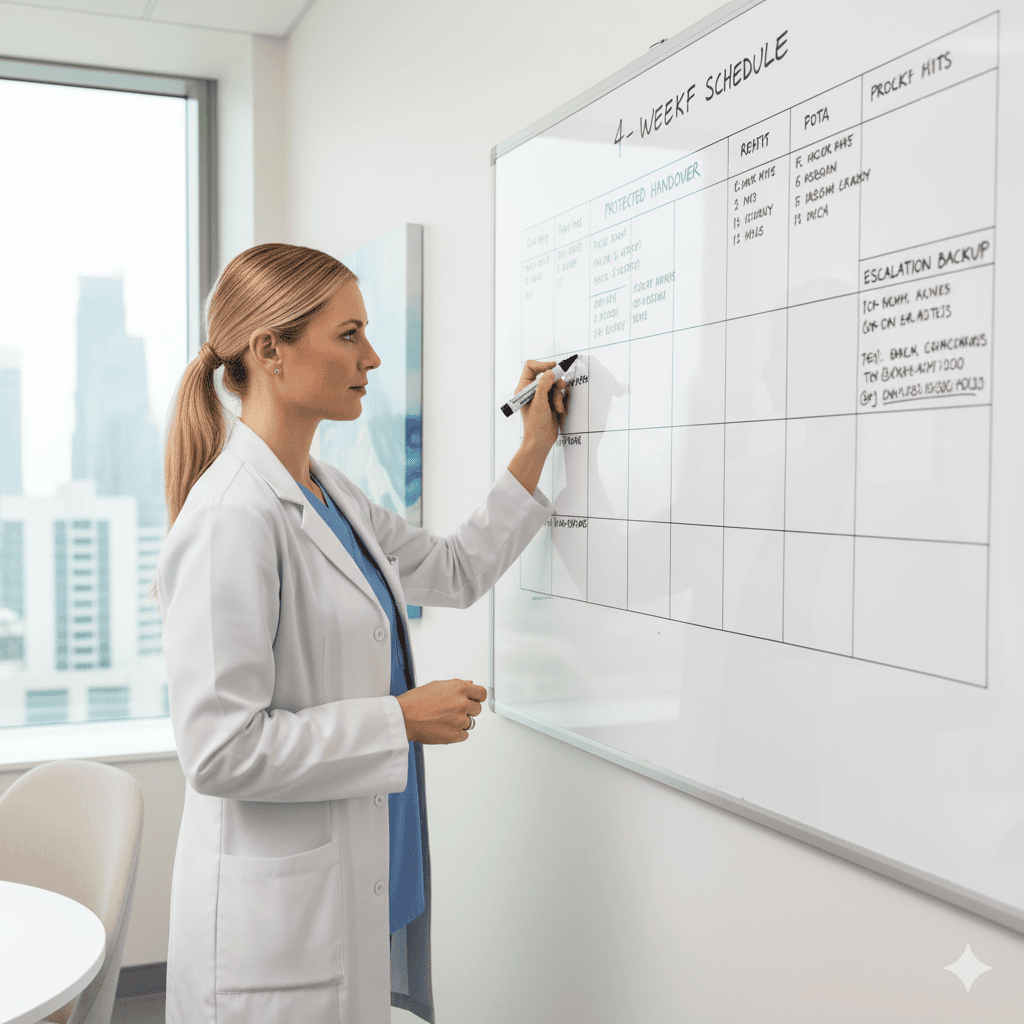
Non-negotiables (copy/paste policy for managers)
Publication window: rota released ≥ 4 weeks in advance; changes documented with reason and approval trail.
Night limits: max 3 consecutive nights, then 1 full post-call day with no clinical duties.
Weekends/holidays: fair rotation logged; no “permanent weekenders.”
Protected handover: 20–30 minutes, no patient flow during this window; attendance tracked.
Escalation cover: named backup for each shift; the escalation tree is visible on the unit board.
Skill mix per shift: at least one senior (or named proctor) present where high-risk procedures or infusions run.
Swap rules: peer-to-peer swaps allowed only if skill mix and rest rules remain intact; manager sign-off required.
Annual leave: request cut-off 6–8 weeks ahead; approved leave locked; surge periods capped.
Safe night duty math (signals, not promises)
ICU/ED/OR: 1 senior + 1–2 associates + clear escalation to on-site consultant/anaesthetist; no solo high-risk coverage.
Inpatient wards: ratio anchored to acuity; night float designated to absorb admissions and reduce interruptions to med-safety tasks.
Clinics/ambulatory: late finishes planned; transport/parking policies set for staff safety; after-hours calls routed to on-call tree.
On-call rules that prevent drift
Caps: maximum X on-call hours/week and Y call-outs/month per grade (define per unit).
Recovery: if call-out > 4 hours between 23:00–06:00, next day switches to admin/education or rest.
Domiciliary/UHNWI: two-person cover for high-risk sessions; travel time counted; household handles logistics only.
Handover standard (SBAR with numbers)
Situation: one-line case ID and current location.
Background: diagnosis, key comorbidities, lines/devices.
Assessment: most recent numeric vitals/score (e.g., SpO₂ 93% on 2 L; pain 7/10).
- Recommendation: explicit escalation thresholds (e.g., MAP <65, SpO₂ <92% for 5 min).Record the time, attendees, and owner of the next action.
Manager’s micro-audits (10 minutes, weekly)
Rota issued ≥ 4 weeks ahead (Yes/No).
Any >3 consecutive nights? (should be 0).
Post-call rest respected (spot-check last week).
Two random handovers contain a numeric escalation line.
Escalation tree posted and accurate for the next 7 days.
Clinic vs hospital nuance
Private clinics (high throughput): rota minimises room turnover pressure—stagger complex procedures; build a clean field pause before sterile packs.
Hospitals: embed proctoring windows for advanced privileges; schedule senior overlap during new hires’ first four weeks.
VIP/UHNWI overlay (privacy without shortcuts)
Keep the same safety rules. Add: discreet transport for late finishes, and a quiet briefing slot with the medical lead after high-profile cases. Household PA/security handle access and transport, never clinical decisions.
What clinicians should ask before accepting a rota
“Is the rota published ≥ 4 weeks ahead?”
“What is the post-call policy?”
“How many consecutive nights are allowed?”
“Who is the escalation backup on each shift?”
“Are domiciliary/UHNWI hours counted and staffed with two clinicians for high-risk sessions?”
Common pitfalls—and calm fixes
Week-to-week rotas → move to 4-week publication; freeze changes 7 days out except for true sickness cover.
Hidden overtime → track call-outs and convert to paid hours or time-off; publish monthly summaries.
No protected handover → lock a 20–30 min slot; patient flow paused; outcomes improve within two weeks.
Skill mix gaps → build a small float team; second senior rotates to highest-risk unit.
Copy-paste checklists
Rota build (manager)
Skill mix per shift verified
Nights capped; post-call days marked
Escalation tree assigned and posted
Proctoring sessions scheduled for new privileges
Domiciliary sessions staffed with two clinicians where required
Weekly review (lead clinician)
Two handovers audited (SBAR + numeric thresholds)
Read-back compliance for high-risk meds observed once
Incident/near-miss huddle completed ≤72 h (if any event occurred)
Fatigue signals checked (sickness spikes, error patterns)
Short FAQs
Discreet contact