Why private clinics need a clinic-grade (not hospital-size) system
Small facilities face high throughput and tight rooms. Risk concentrates at hand hygiene, device reprocessing, and turnover cleaning. A light, visible bundle—owned by the lead clinician—prevents drift and makes standards stick between rooms and shifts.
The core bundle (copy/paste to your clinic wall)
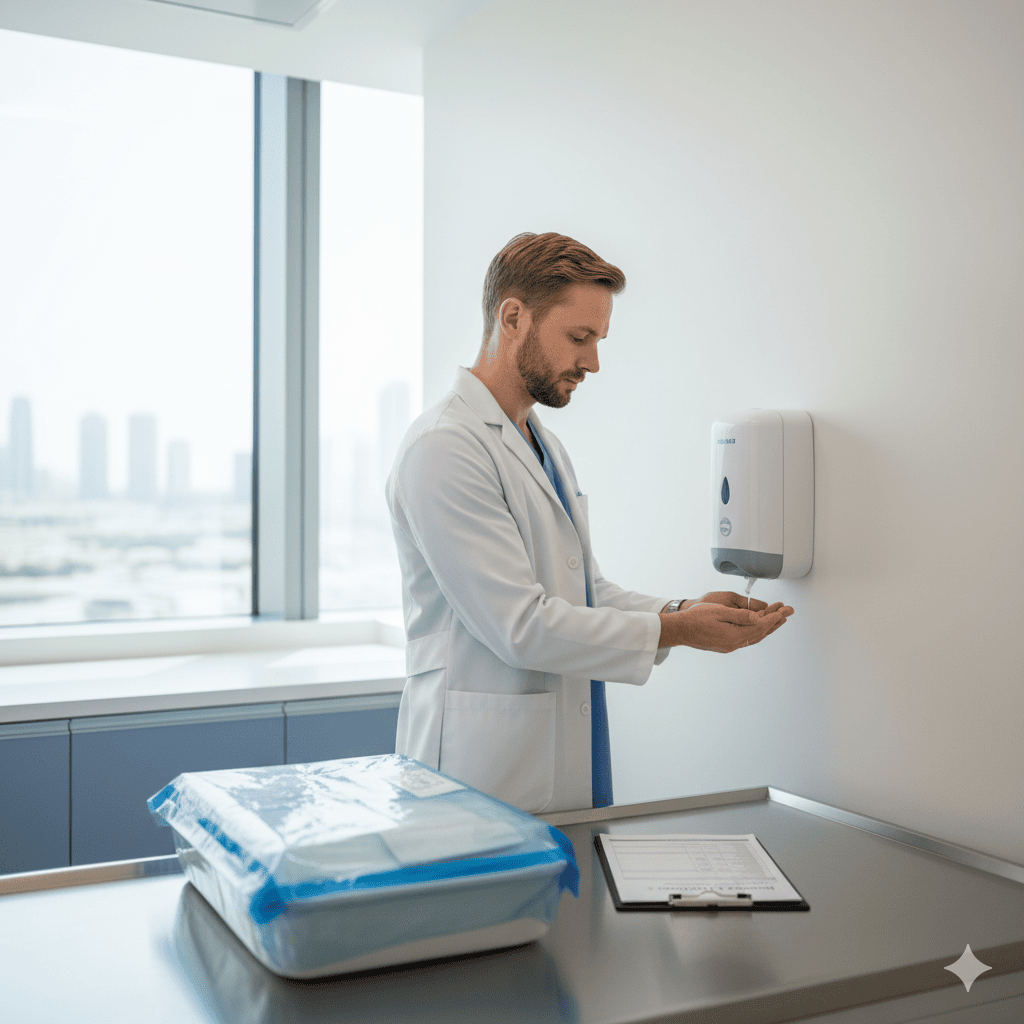
Hand hygiene
5 moments; alcohol rub at every doorway/bed; gloves after, not instead of, hand rub.
PPE
Procedure-appropriate; don/doff sequence posted in each room; single trash path on exit.
Environmental cleaning
High-touch surfaces every patient; terminal clean at day end; log with initials/time.
Device reprocessing
Single-use stays single-use; reusable devices follow manufacturer IFU; traceability sheet per patient.
Sharps & waste
Sharps at eye level, arm’s reach; fill <¾; clinical vs general waste labeled.
Respiratory etiquette & screening
Mask offer at reception for symptomatic patients; isolate or reschedule if needed.
Documentation
One-page room checklist; incident/near-miss form; weekly audit summary.
Patient flow that reduces contamination
Clean-to-dirty direction in rooms; stock on clean side only.
No personal items on clinical surfaces (phones, cups).
Chaperone policy for exams; clear roles so no one breaks clean fields.
Room turnover target time agreed and realistic (quality before speed).
Device & procedure specifics
Point-of-care devices (glucometers, SpO₂): disinfect between patients; change probes/covers.
Ultrasound: single-use gel packets; transducer disinfection per IFU; covers for high-risk sites.
Sterile packs: date/lot recorded; opened immediately before use; discard if field breached.
VIP/UHNWI nuance (privacy without shortcuts)
Same bundle, quieter choreography.
Private waiting area reduces cross-exposure; staff briefed on neutral language in semi-public spaces.
Home/hotel visits: carry a micro-kit (hand rub, wipes, sharps, PPE) and follow the domiciliary SOP.
Role-specific anchors
Five-minute daily micro-audit
ABHR dispensers full and within reach at every room entrance.
Today’s room logs complete and legible.
Sharps bins <¾ full; mounted correctly.
Reusable devices processed with traceability sheet present.
Two random observations of hand hygiene moments documented.
Common pitfalls—and calm fixes
Gloves replace hand rub → retrain; post “gloves are not hand hygiene” reminder at sinks.
Open sterile packs “just in case” → stop; open at point of use only.
Mixed clean/dirty storage → re-shelve; label shelves; place dirty bins away from clean stock.
No time for room turnover → adjust scheduling; quality incidents cost more time.