Why a small bundle beats endless policies
Most avoidable drug events come from look-alike/sound-alike (LASA) confusion, missing double-checks, weight errors and undocumented titrations. A light, visible bundle—owned by the unit lead—reduces noise and protects patients without slowing care.
The high-risk bundle (copy/paste to your unit wall)
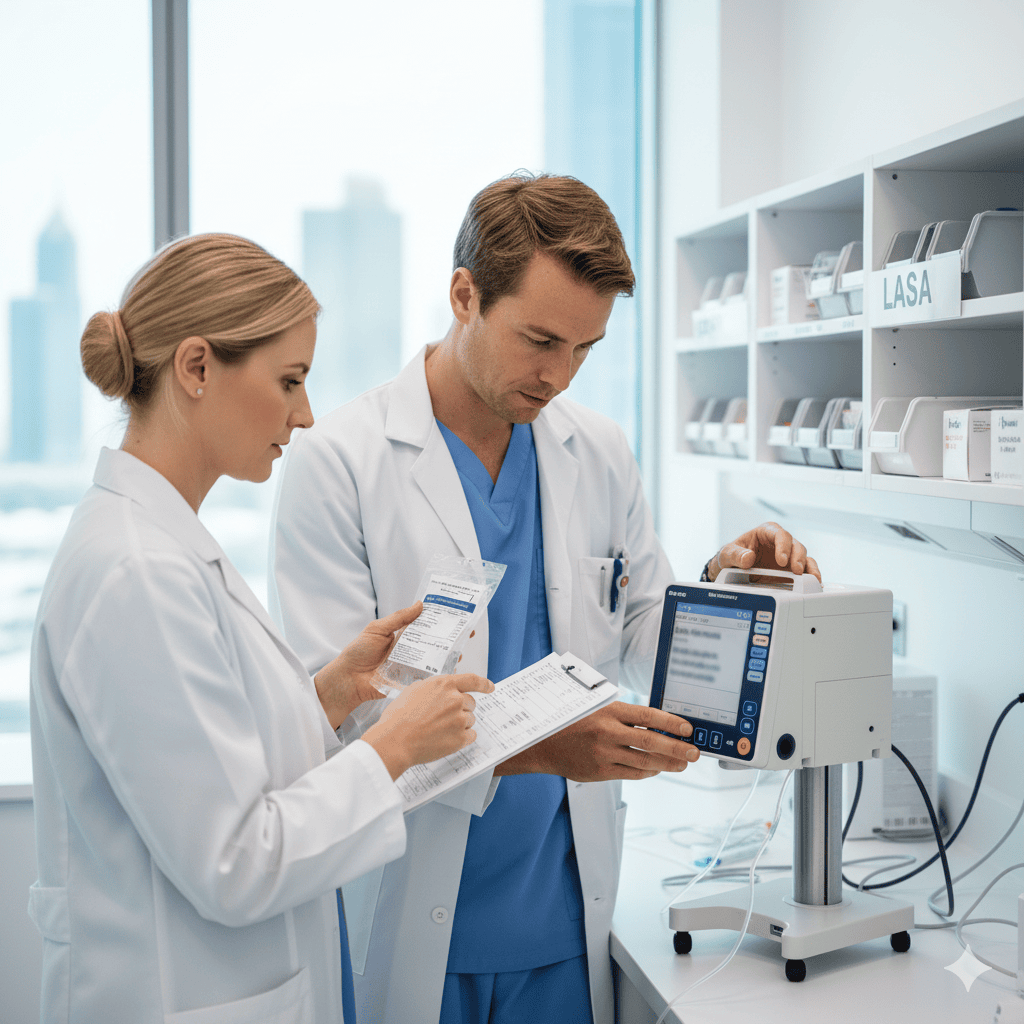
Independent double-check (IDC) before administration
Two clinicians verify drug, dose, route, rate, patient, time—aloud with vial/syringe/pump in view.
LASA read-back
For look-alike/sound-alike pairs, read full names and strengths; store on separate shelves.
Weight & renal line
Document metric weight, date/time, and eGFR where dosing depends on renal function.
Smart-pump library
Use the drug library for all infusions; hard/soft limits active; no “basic mode” for high-risk drugs.
Five-minute pause for new starts
Insulin/anticoagulants/opioids/electrolytes: announce a mini-brief to confirm indication, target, STOP triggers and escalation threshold.
Documentation you can defend
MAR/infusion chart shows indication, starting dose/rate, IDC sign-off, and numeric escalation trigger (e.g., RR>24, MAP<65, SpO₂<92% for 5 min).
Drug-specific anchors (plain English)
Insulin: verify label vs chart, meal timing, IV vs SC; keep hypo kit ready; record CHO plan if relevant.
Anticoagulants (heparin/DOACs/warfarin): note indication (VTE, AF, device), renal function, and reversal plan; avoid duplicate agents.
Concentrated electrolytes (KCl, MgSO₄, Ca): central vs peripheral route rules, dilution and rate; continuous ECG if indicated.
Opioids/PCA: baseline sedation scale, naloxone at hand, co-prescribed laxatives, and explicit hold parameters.
Storage & labelling hygiene
Distinct bins and shelf heights for LASA pairs; never co-locate similar packaging.
Electrolyte concentrates separated from diluents; premix preferred where available.
PCA keys controlled; count at shift change.
VIP/UHNWI nuance (privacy with the same rigor)
Same bundle; quieter choreography. Use neutral descriptors in semi-public areas; update families via the medical lead only.
For home/hotel/yacht visits: carry a domiciliary micro-kit and apply the same IDC and documentation rules.
Role-specific responsibilities
Doctors
Write indication + numeric target/threshold (e.g., aPTT range, pain score, potassium target).
For titrations, prescribe steps and maximum daily change.
Nurses
Enforce IDC and LASA read-backs; use the pump library; document STOP triggers and hand over with SBAR.
Physiotherapists
Before mobilisation, check anticoag status, pain control plan, lines/drains; escalate per thresholds.
Five-item daily micro-audit (takes 4 minutes)
One random IDC observed and signed.
LASA shelves separated and labelled.
Smart-pump infusion found in library mode.
One chart shows weight/eGFR where relevant.
One high-risk case has a numeric escalation line documented.
Common pitfalls—and calm fixes
“We’re busy—skip IDC.” → keep IDC but limit to critical steps; bundle saves time vs managing incidents.
“Basic mode” pumps → lock library use; educate with 10-minute drills.
Weight in pounds → convert to kg and re-document; add a scale-check line to the morning routine.
Electrolytes mixed at bedside → shift to premix or standard dilutions; remove bulk concentrates from general areas.
Short FAQs
Please, talk to David on whatsapp: https://wa.me/34692100254